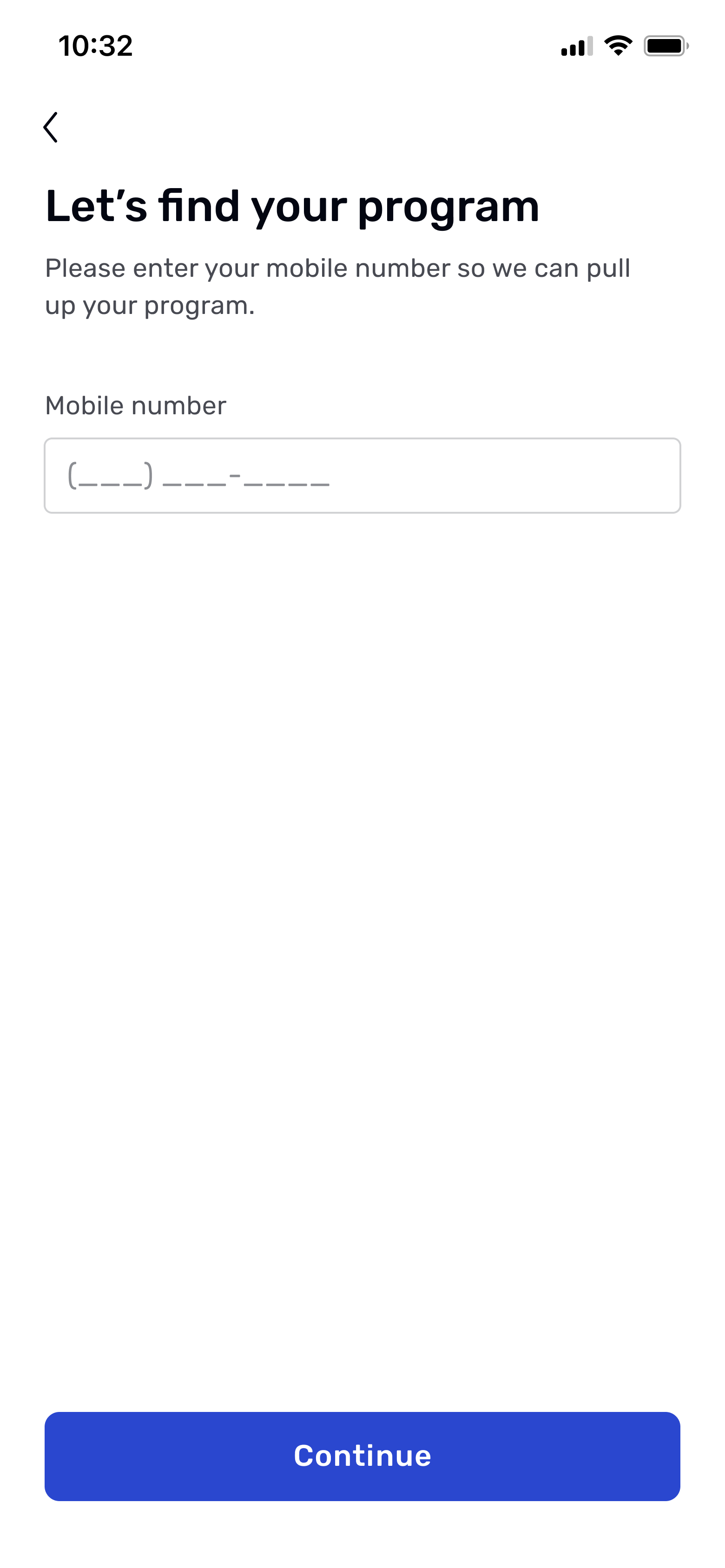
My plan was to focus the next phase of design on instilling confidence in the patient, followed by a phase dedicated to getting them up and running with the app through simple, clear direction.
I began the first phase by testing three different approaches to motivational content to see which resonated most with users:
1. Progress milestones:
Showing patients their projected progress week by week, paired with a simple visual timeline.
2. Success stories from similar patients
Displaying short testimonials from people with similar conditions who saw results by sticking with their exercises.
3. Goal-based motivation
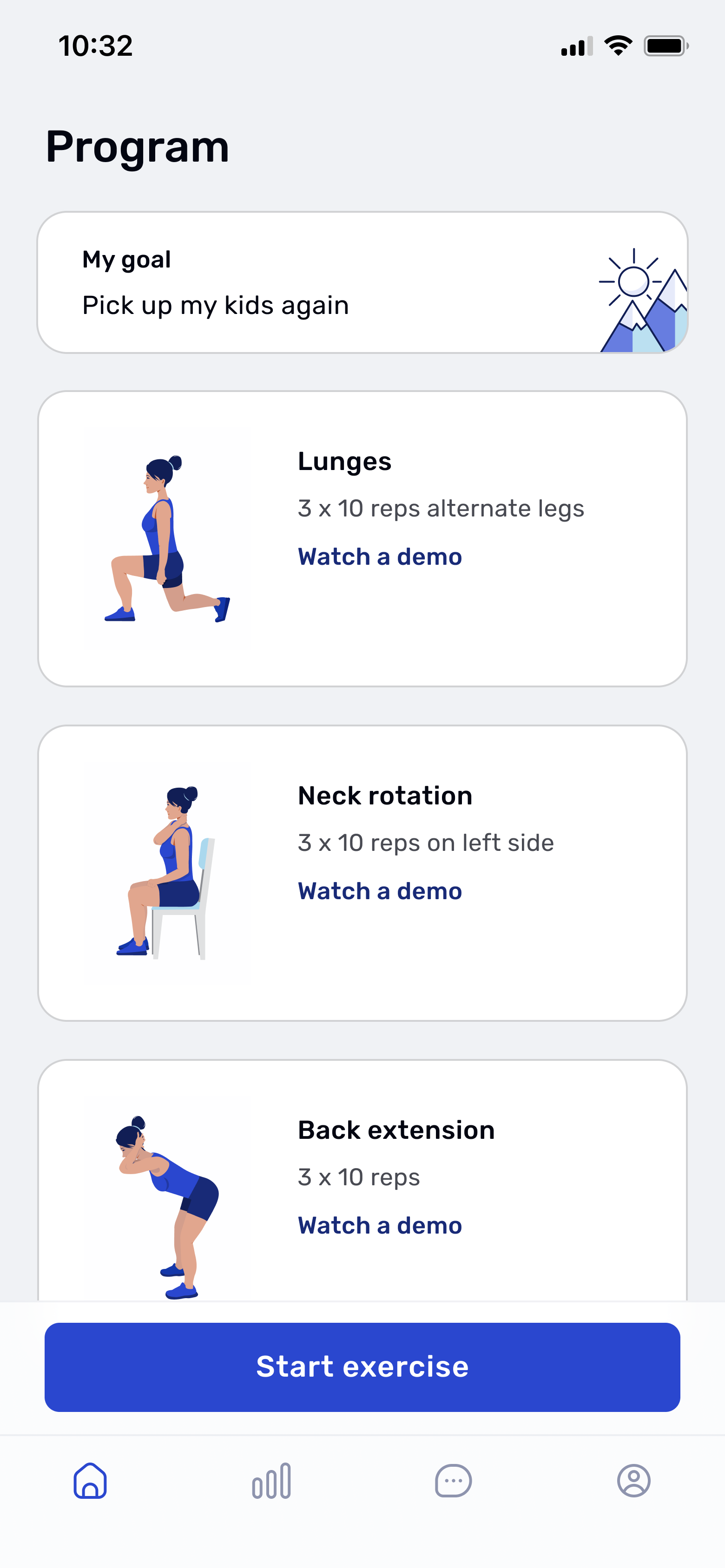
Letting patients set a personal goal, like lifting their child without pain or looking after their home again and do things like cleaning, cooking, and moving around freely. Something they could picture themselves doing but hadn’t been able to since their injury. Then explaining how the assigned exercises would help them reach that goal.
I tested these concepts with 12 users on UserTesting.com, aged 35 to 65, all of whom had prior experience with physical therapy. Most were either employed full-time or retired, with family responsibilities that influenced how they approached time and commitment.
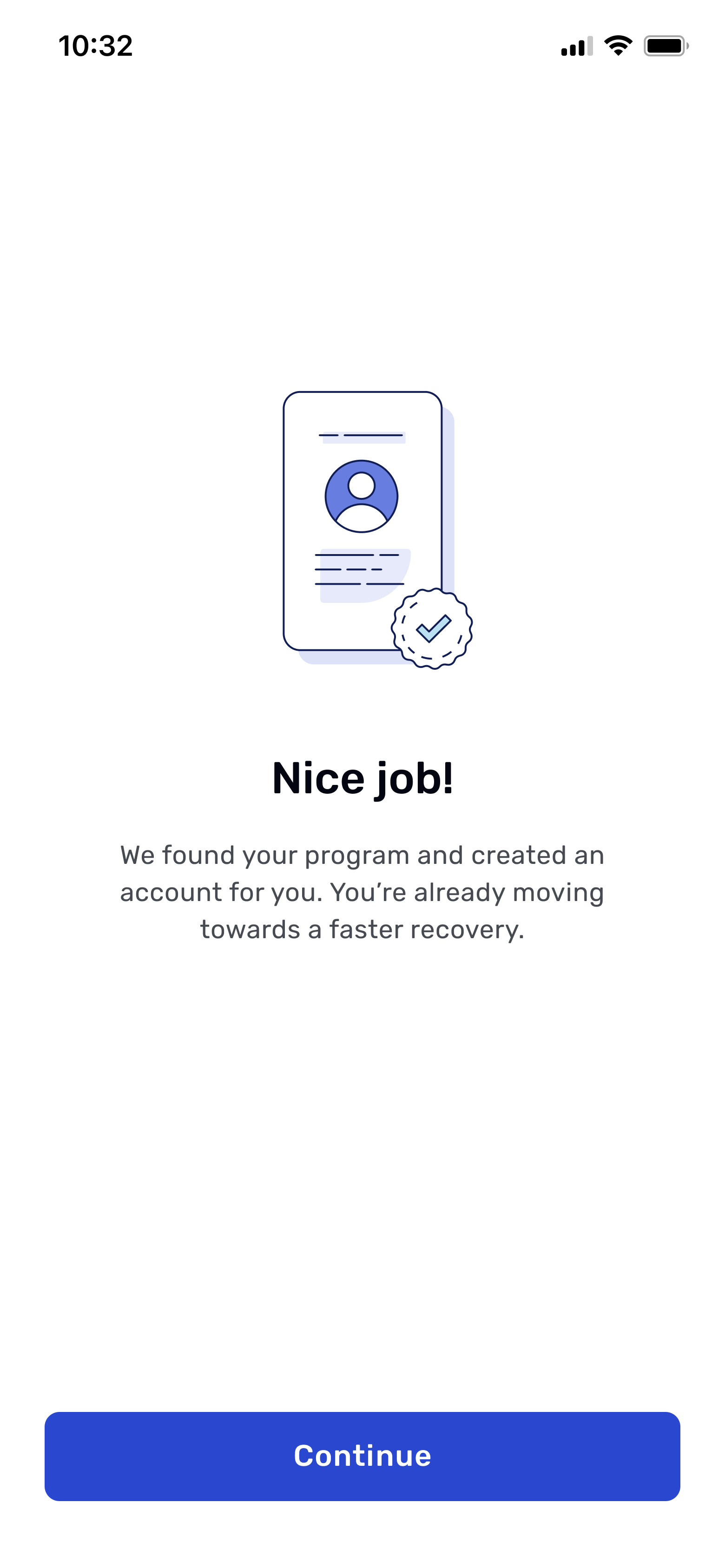
The first two concepts failed to make a strong connection. The clinical milestones were too abstract, and the success stories felt impersonal and dismissible. In contrast, the goal-based concept made a true connection. 83% of testers reacted positively to the idea of working toward something that mattered to them. It gave them a reason to believe in the program and reframed the app as a tool for getting back to the life they wanted.
As one user put it, “It’s good to think about your goal while you’re in the most pain. So that as you’re getting better, you can be reminded of your goal. I like that they’re telling me why I set a goal and that the work I’m doing is all to reach my goal.”
Another said, “Okay, the experience that I just went through was positive and encouraging. And it’s telling me that if I complete this program and I do it properly, I’ll be better. So that is encouraging to me and makes me want to participate. Makes me want to reach my goals.”
With a clear direction established, I ran another round of user testing with 12 new participants to fine-tune content, comprehension, and placement.